Guidelines For Pediatric Myelomeningocele
3. The Management of Patients with Myelomeningocele: Whether Prenatal or Postnatal Closure Affects Future Ambulatory Status
Download pdf Neurosurgery, 2019
Sponsored by: Congress of Neurological Surgeons (CNS) and the Section on Pediatric Neurosurgery
Endorsed by: The Congress of Neurological Surgeons (CNS), American Association of Neurological Surgeons (AANS), and Spina Bifida Association (SBA)
David F. Bauer, MD1, Alexandra D. Beier, DO2, Dimitrios C. Nikas, MD3, Nadege Assassi4, Jeffrey Blount, MD5, Susan R. Durham, MD MS6, Ann Marie Flannery, MD7, Paul Klimo Jr., MD8, Catherine McClung-Smith, MD9, Patricia Rehring, MPH10, Mandeep S. Tamber, MD, PhD11, Rachana Tyagi, MD12, Catherine A. Mazzola, MD13
- Department of Surgery, Division of Neurosurgery, Dartmouth-Hitchcock Medical Center, Lebanon, New Hampshire
- Division of Pediatric Neurosurgery, University of Florida Health Jacksonville, Jacksonville, Florida
- Division of Pediatric Neurosurgery, Advocate Children's Hospital, Oak Lawn, Illinois
- Department of Surgery, Division of Neurosurgery, Robert Wood Johnson Medical School, New Brunswick, New Jersey
- Division of Pediatric Neurosurgery, Department of Neurosurgery, University of Alabama at Birmingham; Children’s of Alabama, Birmingham, Alabama
- University of Vermont, Division of Neurosurgery, Burlington, Vermont
- Kids Specialty Center, Women’s & Children’s Hospital, Lafayette, Louisiana
- Semmes-Murphey; Department of Neurosurgery, University of Tennessee Health Science Center; Le Bonheur Children’s Hospital, Memphis, Tennessee
- Department of Neurological Surgery, Palmetto Health USC Medical Group, Columbia, South Carolina
- Congress of Neurological Surgeons, Schaumburg, Illinois
- Division of Pediatric Neurosurgery, British Columbia Children’s Hospital, University of British Columbia, Vancouver, British Columbia, Canada
- Department of Neurosurgery, Mercer University Medical School, Macon, Georgia
- Goryeb Children’s Hospital, Morristown, New Jersey; Rutgers Department of Neurological Surgery, Newark, New Jersey
Correspondence:
David F. Bauer, MD
Department of Surgery, Division of Neurosurgery,
Dartmouth-Hitchcock Medical Center
Lebanon, New Hampshire
David.F.Bauer@hitchcock.org
Abbreviations:
COI- conflict of interest
MOMS – Management of Myelomeningocele Study
MM – Myelomeningocele
RCT – randomized controlled trial
SB – Spina bifida
TCS – Tethered Cord Syndrome
ABSTRACT
Background: Myelomeningocele (MM) is an open neural tube defect treated by pediatric neurosurgeons with prenatal or postnatal closure.
Objective: The objective of this systematic review was to answer the question: what is the evidence for the effectiveness of prenatal versus postnatal closure of MM regarding short and long-term ambulatory status. Treatment recommendations were provided based on the available evidence.
Methods: The National Library of Medicine PubMed database and Embase were queried using MeSH headings and keywords relevant to ambulatory status after prenatal or postnatal closure of MM. Abstracts were reviewed to identify which studies met the inclusion criteria. An evidence table was assembled summarizing the studies and the quality of evidence (Classes I–III). Based on the quality of the literature, a recommendation was rendered (Level I, II, or III).
Results: One randomized controlled trial (Class II) and 3 retrospective cohort studies (Class III) were included as evidence. Initial ambulatory status depended on anatomic level of the neural tube defect. In the short term, prenatal closure may improve ambulatory status compared to postnatal closure. Spinal cord tethering or dermoid inclusion cyst have been associated with neurologic deterioration in infants closed in utero and after birth. Ambulation may cease in both groups over time. No long-term studies evaluated whether there is a difference in the ability to ambulate upon reaching adulthood.
Conclusions: Prenatal closure of MM may improve ambulatory status in the short term (Level II). Spinal cord tethering in both groups caused deterioration in the ability to walk. Evaluation and treatment of spinal cord tethering may help maintain ambulatory status (Level III). No studies evaluate whether prenatal or postnatal repair provides improved ability to ambulate upon reaching adulthood.
Keywords: Ambulation, evidence, fetal, fetoscopic, in-utero, myelomeningocele, spina bifida
RECOMMENDATIONS
PICO Question: In patients with myelomeningocele, does prenatal or postnatal closure improve the ability to ambulate?
Target Population: Myelomeningocele patients diagnosed prenatally.
Recommendation(s)
- When possible, for prenatally diagnosed fetuses with myelomeningocele who meet maternal and fetal MOMS study inclusion criteria, prenatal closure of myelomeningocele should be performed, which may improve ambulatory status for patients in the short term (at 30 months of age) (Level II).
- Long term benefit for ambulatory status with prenatal closure is unknown. Children who have had either prenatal or postnatal closure should be carefully followed for the development of tethered spinal cord with the associated loss of ambulatory function (Level III).
INTRODUCTION
Rationale
Myelomeningocele (MM), or open neural tube defect, is a condition often diagnosed prenatally with fetal ultrasound or maternal blood test. The current incidence of MM is approximately 3 per 10,000 live births (CDC), with around 1,500 babies born with spina bifida (SB) each year in the United States.1 The incidence was much higher prior to the United States’ government recommendations in 1992 and 1996 to supplement women’s diet with folic acid.1 Historically, postnatal closure was performed to prevent central nervous system infection. With the advent of technology to perform fetal surgery, current options for initial treatment include prenatal and postnatal closure. It is unknown whether there is a benefit for ambulatory status of patients with prenatal versus postnatal closure.
OBJECTIVES
The objective of this systematic review is to evaluate the effect of prenatal closure compared to postnatal closure of the neural placode on the ability to ambulate in patients born with MM. Intended users of these guidelines include medical professionals who treat patients with MM, including providers in the prenatal setting who provide counseling treatment options and those in the postnatal setting regarding prognosis.
METHODS
Writing Group and Question Establishment
The Guidelines Task Force initiated a systematic review of the literature and evidence-based guideline relevant to the diagnosis and treatment of patients with MM. Through objective evaluation of the evidence and transparency in the process of making recommendations, this evidence-based clinical practice guideline was developed for the diagnosis and treatment of patients with MM. These guidelines are developed for educational purposes to assist practitioners in their clinical decision-making processes. Additional information about the methods utilized in this systematic review is provided in the introduction and methodology chapter. The topic of ambulatory status after prenatal or postnatal closure of MM was chosen because of the need to provide better guidance to our patients who present for prenatal counseling for this condition.
Literature Search
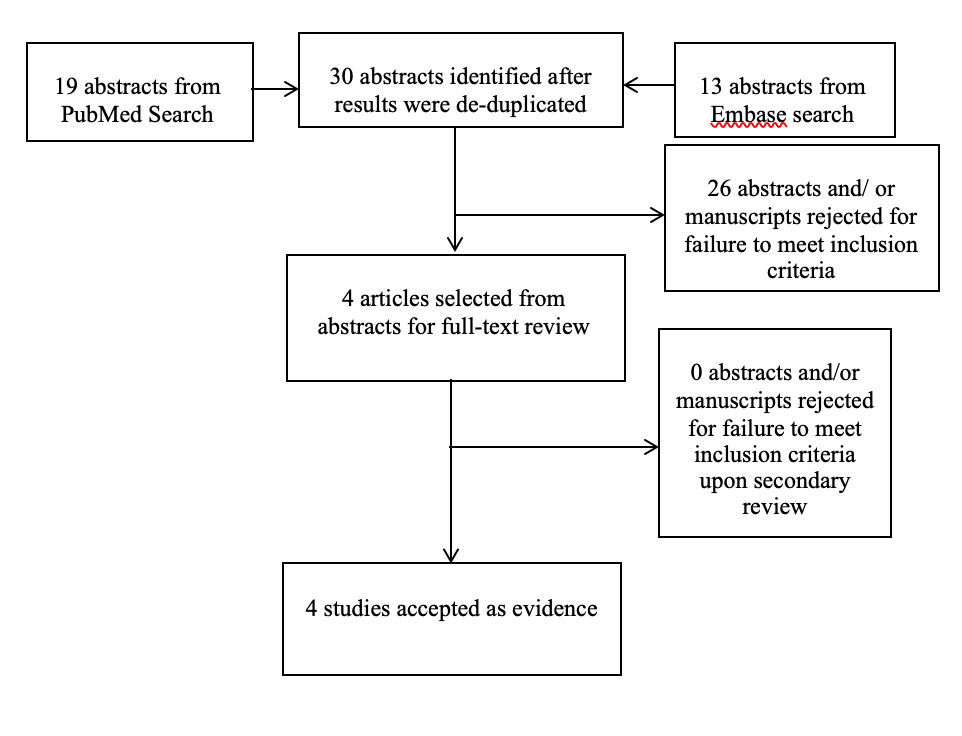
The task force members collaborated with a medical librarian to search the National Library of Medicine PubMed database and Embase for the period from 1966 to September 2016 using the search strategies provided in Appendix I. The literature search yielded 30 abstracts. The task force selected 4 full-text articles for review. Of these, none were rejected for not meeting inclusion criteria or for being off-topic. All 4 articles were selected for systematic review (see Appendix II).2-5
Study Selection and Eligibility Criteria
A total of 30 citations were manually reviewed by the task force with specific inclusion and exclusion criteria as outlined below. Two independent reviewers evaluated and abstracted full-text data for each article, and the 2 sets of data were compared for agreement by a third party. Inconsistencies were re-reviewed, and disagreements were resolved by consensus. Citations that considered pediatric patients with prenatal or postnatal MM closure and evaluated later ambulation status were reviewed. To be included in this guideline, an article must be a report of a study that:
- At least 80% of patients had to be patients with MM and <18 years of age.
- Studies that enrolled >20% of patients with other forms of SB were excluded.
- Studies that combined the results of patients with other forms of SB were excluded if the study enrolled less than 80% of target patient population.
- Studies that enrolled mixed patient populations were included only if they reported separate results for the target population. The results of the target population were the only results considered as evidence to support our recommendations.
- The study was a full article report of a clinical study.
- The study was not a meeting abstract, editorial, letter, or a commentary.
- Prospective case series had to report baseline values, if applicable.
- Case series studies with non-consecutive enrollment of patients were excluded.
- Studies had to have appeared in a peer-reviewed publication or a registry report.
- Studies had to enroll at least 10 patients for each distinct outcome measured. If it was a comparative study, a minimum enrollment of 5 patients per treatment arm for each outcome was necessary.
- The study involved humans.
- The study was published between January 1966 and September 2016.
- The study presented results quantitatively.
- The study did not involve “in vitro”, “biomechanical” or results performed on cadavers.
- The study was published in English.
- Papers reporting results of systematic reviews, meta-analyses, or guidelines developed by others were excluded.
- Authors specifically excluded follow-up studies in which a cohort of patients from an initial study were followed in time and separately reported upon in a subsequent publication. This prevented the same patients from being included multiple times in this review.
The authors did not include systematic reviews, guidelines, or meta-analyses conducted by others.
Data Collection Process
The abstracts that met the selection criteria mentioned above were retrieved in full-text form. Each article’s adherence to the selection criteria was confirmed. To determine how the data could be classified, the information in the full-text articles was then evaluated to determine whether they were providing results of therapy or were more centered on diagnostic or prognostic information. Agreement on these assessments and on the salient points regarding the type of study design and objectives, and the conclusions and data classification was then reached by exchanging drafts and comments by e-mail and discussing questions during monthly phone conference among participants. The information was then used for construction of the evidence tables.
Assessment for Risk of Bias
The literature included in full text review was assessed for risk of bias. The methodological quality of the one randomized controlled trial (RCT) was evaluated using the following 6 criteria: sequence generation, allocation concealment, blinding, incomplete reporting of data, selective reporting of outcomes, and evaluation for other potential threats to validity.
Retrospective case series were assessed for bias by evaluating for selective reporting bias, lack of or loss of information over time, publication bias, bias resulting from a retrospective study, and other types of bias.
Rating Quality of Evidence
The quality of evidence was rated using an evidence hierarchy for 2 different study types; therapeutic and prognostic. Demonstrating the highest degree of clinical certainty, Class I evidence is used to support recommendations of the strongest type, defined as Level I recommendations. Level II recommendations reflect a moderate degree of clinical certainty and are supported by Class II evidence. Level III recommendations denote clinical uncertainty supported by Class III evidence. These hierarchies are shown in Appendix III. Additional information regarding the hierarchy classification of evidence is found here on the CNS Guidelines methodology page.
Revision Plans
In accordance with the Institute of Medicine’s standards for developing clinical practice guidelines, the task force will monitor related publications following the release of this document and will revise the entire document and/or specific sections “if new evidence shows that a recommended intervention causes previously unknown substantial harm; that a new intervention is significantly superior to a previously recommended intervention from an efficacy or harms perspective; or that a recommendation can be applied to new populations.”6 In addition, the task force will confirm within 5 years from the date of publication that the content reflects current clinical practice and the available technologies for prenatal versus postnatal closure of MM.
RESULTS
Study Selection and Characteristics
Literature search found 30 abstracts, 4 of which were chosen for full text review. The other 26 articles were not pertinent to the question or only existed as abstracts. Evaluation of references from these 4 articles found no further primary sources for review. After full text review, all 4 articles were included (see Appendix IV).2-5
Results of Individual Studies, Discussion of Study Limitations and Risk of Bias
Adzick et al.2, published in 2011, provides Class I (primary outcomes) and Class II (secondary outcomes) evidence from a good quality RCT, the Management of Myelomeningocele Study (MOMS). This study randomly assigned eligible women to undergo prenatal surgery at 26 weeks gestational or have standard postnatal repair. Primary outcomes included death, need for CSF shunt by 12 months of age, mental development at 30 months of age scored by the Bayley Mental Development Index, and the difference in anatomic level versus functional level on a motor examination at 30 months of age. A secondary post hoc analysis evaluated the ability to ambulate. Inclusion and exclusion criteria were strict (Appendix V). Inclusion criteria included singleton pregnancy, MM between T1 and S1, evidence of hindbrain herniation, gestational age of 19 to 25.9 weeks at randomization, normal karyotype, US residence, and maternal age 18 years or older. Exclusion criteria included fetal anomaly unrelated to myelomeningocele, severe kyphosis, risk of preterm birth, placental abruption, Body Mass Index of mom of 35 or higher, or contraindication to uterine surgery. Regarding the primary outcome of anatomic level verses functional level, this trial found a significant difference between motor function and anatomic level of 0.58+1.94 in the prenatal group and -0.69+1.99 in the postnatal group. In the post hoc analysis, the authors found that 42% of the prenatal group and 21% of the postnatal group could walk independently without orthotics, 29% of the prenatal group and 36% of the postnatal group could walk with orthotics or devices, and 29% of the prenatal group and 43% of the postnatal group were unable to walk. The MOMS trial was closed early because of the positive treatment effect, therefore 22 postnatal repair and 27 prenatal repair patients were not reported in the article because they were not yet 30 months old at the time of the analysis. A follow up study of these 49 patients with the original cohort was published in 2017.7 This study completed the 30 month outcome analysis on all patients, and found that 44.8% of prenatal patients were independently walking versus only 23.9% of postnatal patients, which are numbers that are similar to the 2011 original analysis. Overall, the study provides Class I evidence for the primary outcome measures. Our PICO question, however, evaluates ambulatory status. This was evaluated in a post hoc analysis. Ambulatory status may relate to lesion level, and to better evaluate ambulatory status the patients should probably have been stratified by lesion level. In addition, the 30 month follow up data was performed on less than 80% of subjects because the study was stopped early, creating potential bias. For these reasons, we believe this evidence should be Class II.
Danzer et al.3 in 2016 provides Class III evidence through a cohort study of MM patients with fetal repair at a single institution prior to the MOMS study. Forty-two of 54 (78%) children who underwent prenatal repair participated in the study, and long-term ambulatory outcomes were assess using a questionnaire because long term in person clinical follow-up was not possible for many patients. At a median of 10 years (range 8-14 years), 33 (79%) were reported as community ambulators, 3 (9%) were reported as household ambulators, and 6 (14%) were wheelchair dependent. Three of 42 patients had spinal cord detethering, all diagnosed in early school years. The need for tethered cord surgery was associate with continued deterioration in ambulatory status.
Williams et al.5 in 1999 provides Class III evidence in a retrospective case series from a single institution of postnatal closure of MM between 1978 and 1993. Data was collected from hospital records detailing annual medical evaluations. The authors investigated the number of patients who could ambulate at some point, and the age at which they began to ambulate and stopped being able to ambulate. Data was presented by level of neural tube defect. One hundred seventy three children were evaluated for their ability to ambulate, with or without assistive devices. Thirty-five children had a thoracic level lesion. Seven walked at mean age 4 years 6 months, and 3 of these children stopped walking at mean age 7 years 6 months. Ten children had a high-lumbar lesion. Five patients walked at mean age 5 years 2 months, and 3 of these patients stopped walking at mean age 6 years 11 months. Fifteen children had mid-lumbar level lesion. Nine patients walked at mean age 5 years, and 3 of these patients stopped walking at mean age 7 years. Forty-five children had low lumbar level lesion. Thirty-eight patients walked at mean age 3 years 10 months, and five of these patients stopped walking at mean age 9 years 1 month. Sixty-eight children had sacral lesions. All patients walked at average age 2 years 2 months, and none had stopped walking at the end of the study period.
Januschek et al.4 in 2016 provides Class III evidence in a retrospective cohort study from a single institution which evaluated outcomes in 48 children with MM (29 patients), meningocele (1 patient), or myeloschisis (18 patients), who were closed between 2007 and 2015. Follow up period ranged between 9 weeks and 8 9/12 years. The authors found that 23 of the 33 patients who were older than age 2 at the time of assessment (70%) were ambulatory with or without orthotic devices at the time of assessment. Four children required spinal cord de-tethering at some point.
DISCUSSION
In this systematic review of the literature, authors found that prenatal closure of MM provided improved motor function level and improved ambulatory status as compared to children who underwent postnatal closure of MM. It is unknown whether these findings are maintained long term due to the potential detrimental effects of future spinal cord tethering in these patients.
The Adzick et al.2 (2011) study found that prenatal closure provided on average a level of function 2 or more levels better than the anatomic level of the neural tube defect. Study patients were more likely to walk without orthotics or other assistive devices. Potential bias comes from lack of randomization of study patients by neural tube defect level and from the post hoc analysis evaluating motor findings, which were not part of the initial outcomes measures. In addition, motor function was evaluated only once at 30 months of age, which limits applying this study to long term ambulatory function in these children. A difference in the rate of re-tethering between cohorts could significantly impact long term ambulatory function.
The Danzer et al.3 (2016) study found that in this cohort of prenatally closed patients, 79% were community ambulators at an average 10 year follow up. This is similar to the 71% of patients in the MOMS study who could ambulate either unassisted or with an assistive device at 30 month follow up. This provides some evidence of the durability of the effect of prenatal closure on ambulatory status. The risk of tethering was 3 of 42 patients (7.1%) which is a similar rate of tethering to other studies in the literature. Bias is assumed because these patients were not followed through skeletal maturity. Patients often exhibit symptoms of tethering during periods of skeletal growth. An average of 10 years follow up misses the teenage years and typical accelerated growth during puberty. If the rate of tethering increases during puberty, this could change this long-term ambulatory status for these patients.
The Williams et al.5 (1999) study found that lower anatomic lesions provided an increased chance a child would be able to ambulate, with or without assistive devices. The study shows that some children may be able to ambulate at a young age, but the child may stop ambulating when the child gets older. The study did not evaluate for reasons for this phenomenon, however the discussion hypothesizes it may include a combination of reasons for a changing body habitus as the child grows older that might prevent ambulation, including weight gain, scoliosis, orthopedic deformity, or even possibly spinal cord tethering. Spinal cord tethering is not specifically addressed in this manuscript. Another potential bias of this study is that the series includes diagnosis of MM, lipomyelomeningocele, and intraspinal lipoma. Another bias is that there was no specific evaluation of the incidence or rate of spinal cord tethering in these patients.
The Januschek et al.4 (2016) study found that 70% of their postnatally closed patients were able to ambulate with or without assistive device at the time of their assessment. This number is higher than the postnatal closure group in the MOMS study,2 however there is potential bias because the assessment was performed retrospectively and there was no specific timepoint when ambulatory status was assessed for every patient. Spinal cord tethering was addressed, and four of the 48 patients (8.3%) underwent spinal cord detething. This number is similar to the rate of tethering described in the Danzer 20163.
Long-term ambulatory status in prenatal closure of MM patients is unknown. Careful clinical follow-up is necessary to evaluate whether prenatal closure of MM has a sustained benefit for improved ambulation. Although tethered cord syndrome (TCS) has developed in some infants who had fetoscopic closure of MM, it is not clear that the rate of development of TCS is higher as compared to infants whose MM was closed after birth. Long-term analysis of gait and functional ambulation should be monitored in all infants with MM.
Future Research
Future research is needed to evaluate whether prenatal closure of MM provides long-term benefit to future ambulatory status. An evaluation of the rate of symptomatic spinal cord tethering in both patient populations would be insightful. A good quality RCT with long-term follow up would be ideal. The authors hope that continued follow-up of the patients from the MOMS trial may answer this question in the future.
CONCLUSIONS
Based on the criteria for the classification of evidence on therapeutic effectiveness (Appendix 3), prenatal closure of MM may improve ambulatory status in the short term (Level II Recommendation). Spinal cord tethering in both groups caused deterioration in the ability to walk. Children who have had either prenatal or postnatal closure should be carefully followed for the development of tethered spinal cord with the associated loss of ambulatory function (Level III Recommendation). No studies evaluate whether prenatal or postnatal repair provides improved ability to ambulate upon reaching adulthood.
Conflict of Interest
The Guidelines Task Force members were required to report all possible conflicts of interest (COIs) prior to beginning work on the guideline, using the COI disclosure form of the AANS/CNS Joint Guidelines Review Committee, including potential COIs that are unrelated to the topic of the guideline. The CNS Guidelines Committee and Guideline Task Force Chair reviewed the disclosures and either approved or disapproved the nomination. The CNS Guidelines Committee and Guideline Task Force Chair are given latitude to approve nominations of Task Force Members with possible conflicts and address this by restricting the writing and reviewing privileges of that person to topics unrelated to the possible COIs. The conflict of interest findings are provided in detail in the companion introduction and methods manuscript.
Disclosures
These evidence-based clinical practice guidelines were funded exclusively by the Congress of Neurological Surgeons, which received no funding from outside commercial sources to support the development of this document.
Disclaimer of Liability
This clinical systematic review and evidence-based guideline was developed by a multidisciplinary physician volunteer task force and serves as an educational tool designed to provide an accurate review of the subject matter covered. These guidelines are disseminated with the understanding that the recommendations by the authors and consultants who have collaborated in their development are not meant to replace the individualized care and treatment advice from a patient's physician(s). If medical advice or assistance is required, the services of a competent physician should be sought. The proposals contained in these guidelines may not be suitable for use in all circumstances. The choice to implement any particular recommendation contained in these guidelines must be made by a managing physician in light of the situation in each particular patient and on the basis of existing resources.
ACKNOWLEDGMENTS
The guidelines task force would like to acknowledge the Congress of Neurological Surgeons Guidelines Committee for their contributions throughout the development of the guideline, the American Association of Neurological Surgeons/Congress of Neurological Surgeons Joint Guidelines Review Committee, as well as the American Academy of Pediatrics, Child Neurology Society and Spina Bifida Association for their review, comments, and suggestions throughout peer review, as well as the contributions of Trish Rehring, MPH, CHES, Senior Manager of Clinical Practice Guidelines for the CNS, and Gretchen Kuntz, MSW, MLIS, for assistance with the literature searches. Throughout the review process, the reviewers and authors were blinded from one another. At this time the guidelines task force would like to acknowledge the following individual peer reviewers for their contributions: Kimon Bekelis, MD; Robin Bowman, MD; Timothy J. Brei, MD; Andrew P. Carlson, MD; John Chi, MD; Mark Dias, MD; Jeffrey Olson, MD; John O’Toole, MD; Michael Partington, MD; Curtis Rozzelle, MD; Krystal Tomei, MD; Jan B. Wollack, MD, PhD.
Appendix I. Search Strategies
| PubMed Strategy |
Results |
Embase Strategy |
Results |
Total Results after De-duplication |
| (((((myelomeningocele[MeSH Terms]) OR myelomeningocele[Text Word])) AND ((spina bifida[MeSH Terms]) OR spina bifida[Text Word])) AND (((((ambulation[Text Word]) OR mobility limitation[MeSH Terms]) OR mobility limitation[Text Word]) OR gait disorders, neurologic[MeSH Terms]) OR neurologic gait disorders[Text Word])) AND ((infant[MeSH Terms]) OR ((((infant[Text Word]) OR prenatal[Text Word]) OR fetal[Text Word]) OR in utero[Text Word])) |
19 |
(('meningomyelocele'/exp OR meningomyelocele) AND ('infant'/exp OR infant OR prenatal OR fetal OR 'in utero') AND ('spinal dysraphism'/exp OR 'spina bifida') AND (ambulation OR 'walking difficulty'/exp OR 'mobility limitation' OR 'neurologic gait disorder'/exp OR 'neurologic gait disorder')) AND [embase]/lim NOT [medline]/lim |
13 |
30 |
Appendix II. PRISMA Article Flow Chart
Appendix III: Rating Evidence Quality
Classification of Evidence on Therapeutic Effectiveness
| Class I Evidence Level I Recommendation |
Evidence from one or more-well designed, randomized controlled clinical trial, including overviews of such trials. |
| Class II Evidence Level II Recommendation |
Evidence from one or more well-designed comparative clinical studies, such as non-randomized cohort studies, case-control studies, and other comparable studies, including less well-designed randomized controlled trials. |
| Class III Evidence Level III Recommendation |
Evidence from case series, comparative studies with historical controls, case reports, and expert opinion, as well as significantly flawed randomized controlled trials. |
Classification of Evidence on Diagnosis
| Class I Evidence Level I Recommendation |
Evidence provided by one or more well-designed clinical studies of a diverse population using a “gold standard” reference test in a blinded evaluation appropriate for the diagnostic applications and enabling the assessment of sensitivity, specificity, positive and negative predictive values, and, where applicable, likelihood ratios. |
| Class II Evidence Level II Recommendation |
Evidence provided by one or more well-designed clinical studies of a restricted population using a “gold standard” reference test in a blinded evaluation appropriate for the diagnostic applications and enabling the assessment of sensitivity, specificity, positive and negative predictive values, and, where applicable, likelihood ratios. |
| Class III Evidence Level III Recommendation |
Evidence provided by expert opinion or studies that do not meet the criteria for the delineation of sensitivity, specificity, positive and negative predictive values, and, where applicable, likelihood ratios. |
Appendix IV. Evidence Table
| Article (Alpha by Author) |
Class of Evidence |
Task Force Conclusions relative to question and rationale for evidence grading |
|
Adzick et al, 20112
|
Class II |
Prospective RCT of 158 patients prospectively randomized to fetal vs postnatal closure of MM. Ambulatory status was evaluated during a post hock analysis. Patients with fetal closure had on average at least two functional levels greater than the anatomic level of the defect. Patients with fetal closure had an increased ability to ambulate at 30 months of age without orthotics than patients with postnatal closure (42% vs 21%, p=0.01). |
|
Danzer et al, 20163
|
Class III |
Retrospective case series of 42 patients who underwent fetal MM closure prior to MOMS study. Ambulation was assessed by questionnaire. Authors concluded that fetal MM surgery improves long-term functional outcome, but spinal cord tethering is associated with functional loss. Authors did not compare patients to postnatal closure cohort. Of the total patients included in the study: 79% community ambulatory, 9% household ambulatory, and 14% wheelchair dependent. |
|
Januschek et al, 20164
|
Class III |
Retrospective case series of 48 patients treated with postnatal closure at a single institution. 23 of 33 patients (70%) over the age of 2 were ambulatory with or without orthosis. Authors believed ambulatory status similar in prenatal and postnatal closure. |
| Williams et al, 19995 |
Class III |
Retrospective case series of 173 patients treated at a single institution over 20 years. 7/35 Thoracic walked, 5/10 high lumbar walked, 9/15 mid lumbar walked, 38/45 low lumbar walked, 68/68 sacral walked. Some children in each group stopped walking over time for reasons not described. Incidence of tethering was not described. |
Appendix V. Major Inclusion/Exclusion Criteria of the MOMS Trial (Adzick et al 2011)
| Inclusion |
- Mothers >18 years of age carrying a singleton pregnancy
- Fetuses with normal karyotype
- Fetuses with a gestational age of 19-25.9 weeks at randomization
- Fetuses with MM defect with an upper level between T1 and S1 with evidence of hindbrain herniation
|
| Exclusion |
- Fetuses with a severe kyphotic deformity related to MM
- Fetuses with a fetal anomaly unrelated to MM
- Risk of preterm birth, placental abruption or any other contraindication to surgery.
- Mother with Body Mass Index of >35
|
REFERENCES
- Centers for Disease Control and Prevention. Data & Statistics on Spina Bifida. 2018; https://www.cdc.gov/ncbddd/spinabifida/data.html. Accessed December 31, 2018.
- Adzick NS, Thom EA, Spong CY, et al. A randomized trial of prenatal versus postnatal repair of myelomeningocele. N. Engl. J. Med. Mar 17 2011;364(11):993-1004.
- Danzer E, Thomas NH, Thomas A, et al. Long-term neurofunctional outcome, executive functioning, and behavioral adaptive skills following fetal myelomeningocele surgery. Am. J. Obstet. Gynecol. Feb 2016;214(2):269 e261-269 e268.
- Januschek E, Rohrig A, Kunze S, Fremerey C, Wiebe B, Messing-Junger M. Myelomeningocele - a single institute analysis of the years 2007 to 2015. Childs Nerv. Syst. Jul 2016;32(7):1281-1287.
- Williams EN, Broughton NS, Menelaus MB. Age-related walking in children with spina bifida. Dev. Med. Child Neurol. Jul 1999;41(7):446-449.
- Ransohoff DF, Pignone M, Sox HC. How to decide whether a clinical practice guideline is trustworthy. JAMA. Jan 9 2013;309(2):139-140.
- Farmer DL, Thom EA, Brock JW, 3rd, et al. The Management of Myelomeningocele Study: full cohort 30-month pediatric outcomes. Am. J. Obstet. Gynecol. Feb 2018;218(2):256 e251-256 e213.