Reposted with permission from ©AANS, 2014
J Neurosurg Pediatrics (Suppl) 14:30–34, 2014
AANS, 2014
(Original text of the guideline was edited to reflect the update. Please click here for the original publication.)
Pediatric hydrocephalus: systematic literature review and evidence-based guidelines
Part 4: Cerebrospinal fluid shunt or endoscopic third ventriculostomy for the treatment of hydrocephalus in children
UPDATE
David Dr. Limbrick Jr., MD, PhD,1 Lissa C. Baird, MD,2Paul Klimo Jr., MD, MPH,3-5 Jay Riva-Cambrin, MD, MSc,6 Ann Marie Flannery, MD7
1Division of Pediatric Neurosurgery, Department of Neurological Surgery, Washington University School of Medicine, St. Louis, Missouri; 2Department of Neurological Surgery, Oregon Health & Science University, Portland, Oregon; 3Semmes-Murphey Neurologic & Spine Institute, 4Department of Neurosurgery, University of Tennessee Health Science Center, and 5Le Bonheur Children’s Hospital, Memphis, Tennessee; 6Division of Pediatric Neurosurgery, University of Utah School of Medicine, Salt Lake City, Utah; 7Department of Neurological Surgery, Saint Louis University, St. Louis, Missouri
Object. The objective of this systematic review was to examine the existing literature comparing CSF shunts and endoscopic third ventriculostomy (ETV) for the treatment of pediatric hydrocephalus and to make evidence-based recommendations regarding the selection of surgical technique for this condition.
Methods. Both the US National Library of Medicine and the Cochrane Database of Systematic Reviews were queried using MeSH headings and key words specifically chosen to identify published articles detailing the use of CSF shunts and ETV for the treatment of pediatric hydrocephalus. Articles meeting specific criteria that had been determined a priori were examined, and data were abstracted and compiled in evidentiary tables. These data were then analyzed by the Pediatric Hydrocephalus Systematic Review and Evidence-Based Guidelines Task Force to consider treatment recommendations based on the evidence.
Results. Of the 122 articles identified using optimized search parameters, 52 were recalled for full-text review. One additional article, originally not retrieved in the search, was also reviewed. Fourteen articles met all study criteria and contained comparative data on CSF shunts and ETV. In total, 6 articles (1 Class II and 5 Class III) were accepted for inclusion in the evidentiary table; 8 articles were excluded for various reasons. The tabulated evidence supported the evaluation of CSF shunts versus ETV.
Conclusions. Cerebrospinal fluid shunts and ETV demonstrated equivalent outcomes in the clinical etiologies studied.
Recommendation: Both CSF shunts and ETV are options in the treatment of pediatric hydrocephalus. Strength of Recommendation: Level II, moderate clinical certainty.
(http://thejns.org/doi/abs/10.3171/2014.7.PEDS14324)
Key Words: hydrocephalus, cerebrospinal fluid, ventriculoperitoneal, shunt, endoscopic third ventriculostomy, practice guidelines
Abbreviations used in this paper: AANS = American Association of Neurological Surgeons; CNS = Congress of Neurological Sur- geons; CPC = choroid plexus cauterization; ETV = endoscopic third ventriculostomy; VP = ventriculoperitoneal.
Selection of the appropriate surgical method—CSF shunt placement or endoscopic third ventriculostomy (ETV)—for the treatment of pediatric hydrocephalus remains a topic of considerable debate. Advocates for ETV cite low failure rates and the potential to avoid shunt placement and its inherent risks as major advantages of the procedure, while supporters of insertion of a ventriculoperitoneal (VP) shunt question the efficacy of ETV in treating hydrocephalus as well as ETV’s unknown effects on neurodevelopment and quality of life.1-3 While there is a great deal of literature on CSF shunts and ETV, there is a relative dearth of articles describing evaluation of both CSF shunt placement and ETV, and there are no randomized trials in which the 2 procedures have been compared.
Endoscopic third ventriculostomy may be beneficial in cases in which there is a clear obstruction to CSF flow and ETV provides an alternate pathway. It is less certain that ETV holds an advantage over shunts in many other causes of hydrocephalus. There is a great deal of interest in the use of ETV with choroid plexus coagulation (CPC) in the treatment of infant hydrocephalus. The Pediatric Hydrocephalus Systematic Review and Evidence-Based Guidelines Task Force anticipates that this topic, along with the effectiveness of ETV compared with shunts in treating hydrocephalus of specific etiologies, will be addressed in subsequent publications. In the current analysis, we sought to systematically review the existing literature detailing the efficacy of CSF shunts versus ETV and to generate evidence-based recommendations for the selection of surgical procedure based on the strength of the available data. Evidence for ETV and a discussion of that procedure in infants younger than 1 year of age is addressed elsewhere in the Guidelines.4
The primary objective of this work was to broadly assess treatment outcomes and review evidence that one treatment may have greater efficacy than the other.
Methods
Search Criteria
The US National Library of Medicine PubMed/ MEDLINE database and the Cochrane Database of Sys- tematic Reviews were queried using MeSH headings, key words, and terms relevant to hydrocephalus, CSF shunts, and ETV. The structure of the literature queries used to search these databases for published articles relevant to hydrocephalus, CSF shunts, and ETV is explained below and in “Part 1: Introduction and Methods.”5
Search Terms
PubMed/MEDLINE
- ((“Hydrocephalus”[Majr]) AND “Ventriculosto- my”[Majr]) AND “Endoscopy”[Mesh]
- Limit 1 to Child (0–18 years)
- Limit to English and Humans Number = 120
Cochrane Database
- MeSH descriptor Child
- MeSH descriptor Infant
- MeSH descriptor Hydrocephalus
- MeSH descriptor Ventriculostomy
- MeSH descriptor Third Ventricle
- (1 or 2) and 3 and 4
- (1 or 2) and 3 and 5
Number = 2 Systematic Reviews
Abstracts of papers that were identified using these optimized search parameters (n = 122) were screened for inclusion criteria. Electronic searches were supplemented by manual searches of article bibliographies. Of the 122 records that were screened, 52 articles were recalled for a full-text review. One additional article identified but not retrieved in the search was also reviewed. Fourteen articles contained comparative data on CSF shunts and ETV, a criterion defined a priori for the current study. Please refer to Part 1 of the Guidelines,5 which offers additional inclusion/exclusion criteria and search terms that were used.
Authors performed an updated literature search (in PubMed and Cochrane Central) for this guideline chapter through a medical librarian at the Congress of Neurological Surgeons Guidelines office using the below-mentioned existing search terms to update the original search through November 30, 2019, yielding an additional 107 abstracts. Of those, 22 were screened for full text review.
Search Strategy
An evidentiary table was constructed to facilitate data review and analysis by the Task Force. Each of the 14 articles was read and reviewed in detail by the full Task Force. Afterward 7 articles were excluded due to potential redundancy in the subject population (n = 3), potential redundancy and variable or inappropriate outcome measures (n = 2), or a clinical scenario in which hydrocephalus might reasonably be expected to resolve without ETV or shunt surgery (n = 2); and 1 article was excluded because it covered simultaneous treatment with a CSF shunt and ETV (Fig. 1).6-13 The evidentiary table was constructed to link recommendations to strengths of evidence (Levels I–III), which were assigned by a group consensus during face-to-face meetings of the Task Force.
Part 4 explores the utility of ventriculoperitoneal shunt (VPS) placement versus endoscopic third ventriculostomy (ETV) for children with hydrocephalus. Twelve new studies out of 107 abstracts resulting from this review met inclusion criteria as described in the original guideline. Of those, nine studies affirmed the previous recommendation stating that VPS and ETV are both options for the treatment of HC in children (Level II).
Search Results
Of the 122 articles identified using the optimized search parameters, 52 were recalled for full-text review. Members of the Task Force who were assigned to the current topic read and discussed all 52 articles recalled for the full-text review as well as the additional study identified and subsequently disqualified. As the primary objective of this study was to assess treatment outcomes following placement of a CSF shunt or ETV, the scope of the evidentiary review was limited to studies that reported quantitative outcomes on both procedures (n = 14). In total, 6 articles (1 Class II and 5 Class III) were accepted for inclusion in the evidentiary table (Table 1)14-19 and 8 were excluded for various reasons as detailed above.6-13 When more than 1 paper covered the same clinical material or included the same subjects, only the paper with the largest patient population and most current data was included in the evidentiary table. The tabulated evidence provided adequate data to allow our evaluation of CSF shunts versus ETV.
Two articles6,8 were excluded because they contained redundant material or constituted duplicate publication. When more than 1 paper covered the same clinical material, only the paper with the largest patient population and most current data was included in Table 1 as evidence to support the topic. Two other articles by the same group of researchers were also excluded: one because of possible subject redundancy and insufficient data to address the primary objective,9 and the other because it contained differing outcome measures.10 Two articles were excluded because they evaluated the role of ETV11 or ETV and CSF shunts7 prior to posterior fossa surgery for tumor excision, a clinical scenario in which hydrocephalus may reasonably be expected to resolve in some cases. Finally, 1 article was excluded because its topic was simultaneous ETV and CSF shunt implantation, which prohibited an assessment of the outcome of either procedure alone.12
The 2020 update yielded 107 abstracts, of which, 22 were selected for full text review and 6 new studies met inclusion criteria as described above.
Results
Recommendation: Both CSF shunts and ETV are options in the treatment of pediatric hydrocephalus. Strength of Recommendation: Level II, moderate clinical certainty.
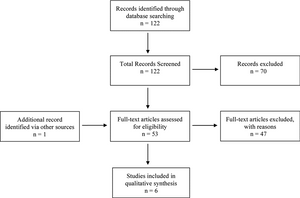
Fig. 1. Flowchart showing the process involved in identifying relevant literature. See text for exclusion criteria at each stage.
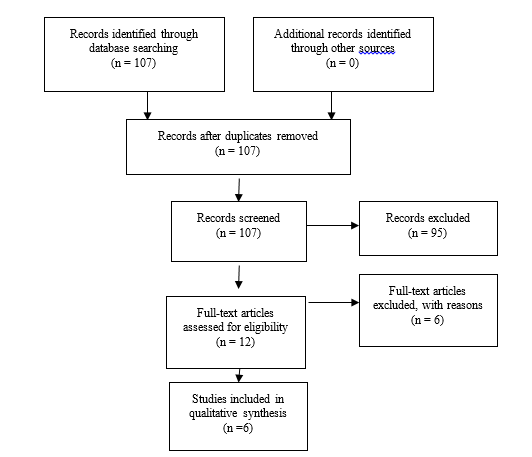
Fig. 2. Flowchart showing the process involved in identifying relevant literature for the 2020 Update. The criteria for “records excluded” and “full text articles excluded with reasons” are detailed in Part 1 of the Guidelines.
Cerebrospinal fluid shunts and ETV demonstrated equivalent outcomes in the clinical scenarios that were studied.
All relevant articles, including those planned for inclusion and exclusion, were reviewed before finalizing the evidentiary table. Each article was presented and discussed in detail, and careful deliberation was made to determine each article’s data class. In sum, there were 5 Class III articles and 1 Class II article (Table 1).
Tuli et al. (1999) published the sole article included in the evidentiary table rated as Class II.19 The authors reported results from a single-center, nonrandomized, prospective cohort study investigating outcomes in 242 consecutive patients treated with ETV (n = 32) or VP shunts (n= 210). While differences in patient ages and the etiology of hydrocephalus were noted among groups (patients who underwent ETV were older at surgery and more likely to have aqueductal stenosis), no significant difference was observed in the procedure failure rate, with a 44% failure rate for ETV and a 45% failure rate for VP shunt surgery.
The remaining 5 articles included in the evidentiary table were rated as Class III studies. Appelgren and colleagues14 (2010) reported a retrospective analysis of prospectively acquired data in 98 patients treated with VP shunts (76 patients) or ETV (22 patients). The primary outcome was failure of the surgery, which was recorded when subsequent surgery was required. Failure rates for VP shunt surgery and ETV were 58% and 55%, respectively, with a mean follow-up of 4.7 years. Study group allocation was uncontrolled, and there was variability in patient ages at surgery, the etiology of hydrocephalus, and other factors.
De Ribaupierre et al.15 (2007) reported the results of a retrospective review of 55 procedures (24 ETVs and 31 VP shunt placements) performed in 48 patients in the context of a literature review. With a median follow-up of 39 months, the authors noted a trend toward a lower failure rate in the ETV group (26% vs 42% in the VP shunt group), although this was not significant. The authors acknowledged nonsignificant differences in patient age and sex as well as in the etiology of hydrocephalus among their groups. Shimizu et al.18 (2012) presented a retrospective, 2-center review of cases in which ETV (9 patients) or VP shunt surgery (36 patients) was performed after removal of infected shunts. No significant difference was observed between the 2 groups in reinfection rates or procedural longevity. Of note, however, 7 of the 9 ETVs ultimately failed in this case series of patients being treated after shunt infection.
Garton et al.16 (2002) reported a retrospective, single- institution, matched cohort study in which ETV was com- pared with VP shunt surgery. With 28 patients in each group, no significant differences were noted between the 2 procedures in the treatment success rate or in cost-effectiveness parameters such as length of stay, operating time, or cost per patient. The authors acknowledge several limitations in this study, including modest sample sizes, a long treatment interval with practice deviation over time, and the possibility of missing late ETV failures (there was 1 hydrocephalus-related death in this group).
The largest study included in the evidentiary table was conducted by Kulkarni et al.8 (2010). This large multicenter comparative study had 2 arms: a retrospective arm for ETV (n = 489), and an arm in which prospectively acquired data for VP shunts was obtained from 2 previous clinical trials and reanalyzed for this study (n = 720). As noted previously, several related studies by the same research group were excluded, because there was likely overlap in the patients included in these studies. Although this paper was rated by the Task Force as Class III, Kulkarni et al. described a sophisticated analysis of ETV versus VP shunt surgery on a large scale. The initial unadjusted models showed lower rates of failure for ETV compared with shunt surgery, but when adjusted for patient age and hydrocephalus etiology, the comparison became more complicated: early failure was higher for ETV than for shunt placement, but at points after 3 months, the ETV failure rate was lower than that for shunt surgery. Based on these findings, the authors concluded that there may be a long-term treatment survival advantage for ETV.
Ultimately, there are a number of limitations to this systematic review. In narrowing the scope of this project to focus specifically on evaluating the method of hydrocephalus treatment—VP shunt or ETV—several key factors known to impact the success of ETV, namely patient age, etiology of hydrocephalus, and history of prior hydrocephalus surgery, were not assessed.8 Thus, the heterogeneity in subject data that we have analyzed herein inherently limits the ability of this recommendation to inform surgical decision making in any specific case. Further, emerging information regarding the role of choroid plexus cauterization (CPC) in conjunction with ETV and alternative indications for ETV with or without CPC (for example, posthemorrhagic hydrocephalus of prematurity) should be evaluated in future iterations of guidelines for the treatment of hydrocephalus as more information becomes available.13 Finally, and most significantly, there is an urgent need for large-scale randomized controlled trials to generate the Level I evidence that is required to definitively address the question of the optimal surgical technique (VP shunt, ETV, or ETV-CPC) in cases of any given hydrocephalus etiology.
2020 Update
Six studies20-25 affirmed the previous recommendation stating that VPS and ETV are both options for the treatment of HC in children (Level II).
Conclusions
Recommendation: Both CSF shunts and endoscopic third ventriculostomy (ETV) are options in the treatment of pediatric hydrocephalus. Strength of Recommendation: Level II, moderate clinical certainty.
Cerebrospinal fluid shunts and ETV demonstrated equivalent outcomes in the clinical scenarios that were studied.
Acknowledgments
We acknowledge the American Association of Neurological Surgeons (AANS)/Congress of Neurological Surgeons (CNS) Joint Guidelines Committee for the members’ reviews, comments, and suggestions; Laura Mitchell, Guidelines Project Manager for the CNS, for her contributions; Pamela Shaw, research librarian, for her assistance with the literature searches; Kevin Boyer for his assistance with data analysis; and Sue Ann Kawecki for her assistance with editing. We also acknowledge the following peer reviewers for their contributions to review the update to the guidelines: Jennifer Sweet, MD, Brandon Rocque, MD, Christoph Greissenauer, MD, Jeffrey Olson, MD.
Disclosure
Dr. Limbrick receives research funding through the National Institute of Neurological Disorders and Stroke. The systematic review and evidence-based guidelines were funded exclusively by the CNS and AANS Pediatric Section, which received no funding from outside commercial sources to support the development of this document.
Conflict(s) of Interest: None. All Task Force members declared any potential conflicts of interest prior to beginning work on this evidence review.
Conflict(s) of Interest: None. All Pediatric Hydrocephalus Systematic Review and Evidence-Based Guidelines Update Task Force members declared any potential conflicts of interest prior to beginning work on this systematic review and evidence-based guidelines.
Author contributions to the study and manuscript preparation include the following. Conception and design: AANS/CNS Joint Section on Pediatrics. Acquisition of data: all authors. Analysis and interpretation of data: all authors. Drafting the article: Limbrick. Critically revising the article: all authors. Reviewed submitted version of manuscript: all authors. Approved the final version of the manuscript on behalf of all authors: Flannery. Administrative/technical/ material support: all authors. Study supervision: Flannery.
Evidence Tables
Table 1 Evidentiary Table Evaluating CSF shunts and ETV
| First Author & Year |
Study Description |
Data Class, Quality and Reasons |
Results and Conclusions |
|
Tuli S et al., 1999
|
Single center, non-randomized, prospective cohort study. Analyzed all subjects over 10 year period with hydrocephalus from AS or tumor.
|
Class II
Prospective cohort study of consecutive subjects
|
32 ETV, 210 VPS patients: 14 (44%) and 95 (45%) failed, respectively. ETV patients were older (median age = 8.1 vs. 3.6 years) and had a higher incidence of aqueductal stenosis (53 vs. 25%). No Difference observed among groups (p = 0.66, hazard ratio = 1.19, 95% confidence interval = 0.55-2.56). |
|
Appelgren et al., 2010
|
Retrospective analysis of a prospective case series of
98 subjects treated with VP shunt or ETV. Primary outcome: procedure failure for VP shunt or ETV. Time to failure also noted. |
Class III
Retrospective analysis of an uncontrolled, prospective case series
|
Failure: ETV 55%, VPS 58%. Hazard ratios calculated for failure of shunts, prematurity, and length of procedure. Variability present in age, etiology of hydrocephalus, and other factors.
|
|
|
de Ribaupierre S et al., 2007
|
Retrospective review of 55 procedures in 48 consecutive subjects (24 ETVs, 31 VP shunts).
|
Class III
Retrospective review
|
Difference in failure rate not significant (26% with ETV versus 42% with VP shunt)
No difference between groups at 6 months,1 year, 2 years, or 5 years after surgery. |
|
Garton et al., 2002
|
Matched cohort analysis of ETV vs. VP shunt with comparison of cost-effectiveness and procedure failure rate. n=28 for both groups.
|
Class III
Retrospective single-institution matched cohort study. The study interval was prolonged (10 years) and contained practice variation.
|
ETV success rate of 54% was not significantly different than VP shunt. However, at 34 months post-op, the procedure survival curve favored ETV. No difference between procedures observed in cost or efficacy. |
|
|
Kulkarni et al., 2010
|
International, multicenter study comparing retrospective data for ETV and prospectively-acquired data for shunts (from the Shunt Design Trial and the Endoscopic Shunt insertion Trial). Primary outcome: treatment failure, defined as any subsequent surgical procedure for CSF diversion or death related to hydrocephalus management.
|
Class III
Multicenter comparative study with two arms: 1) retrospective for ETV; 2) prospectively-acquired data from 2 previous trials re-analyzed in the current study.
|
Unadjusted models showed lower rates of failure for ETV compared to shunting. After adjusting for age and hydrocephalus etiology, early failure was higher in ETV than shunting; however, at points after 3 months post-surgery, ETV failure was lower than shunting. Conclusion: the risk of ETV failure is initially higher than shunting, but after 3 months, the risk of ETV failure is less than shunt failure. |
|
|
Shimizu et al., 2012
|
Retrospective, two-center study of ETV (n=9) or VP shunt (n=36) after removal of infected VP shunt. Compared re-infection rates after each procedure and procedure longevity.
|
Class III
Retrospective review, modest sample size.
|
Reinfection rates were not significantly different between VP shunt (27.8%) and ETV (11.1%). Procedure longevity not different between VP shunt (658 days) and ETV (929 days). |
|
Table 2. New evidence included in 2020 Update
| First Author & Year |
Study Description |
Data Class, Quality and Reasons |
Results and Conclusions |
|
Fani et al, 2013
|
Study of children under 2 years with hydrocephalus undergoing ETV
|
III
|
Shows no significance resulting from the use of ETV. |
|
Jernigan et al, 2014
|
Multi-center retrospective cohort study of infants comparing ETV to VPS.
|
III
|
This study showed failure rates were higher in ETV than VPS.
|
|
|
Kalkarni et al, 2014
|
Retrospective, multicenter cohort study of children under age 2 with ETV-CPC versus VPS.
|
III
|
ETV- CPC in infants is reasonably safe in certain scenarios. The degree of CPC may be associated with surgeon experience.
|
|
Lam et al, 2014
|
Retrospective multicenter study of children with ETV
|
III
|
ETV success was higher in children age 1 year or older and without any prior shunts. |
|
Stone et al, 2014
|
Prospective study of infants under 2 treated with ETV CPC
|
III
|
In this population (North American), ETV-CPC is a safe and effective treatment for hydrocephalus in infants.
|
|
Vogel et al, 2013
|
Retrospective single center study of ETV in children
|
III
|
ETV is effective and safe in certain patents with hydrocephalus. When ETV is successful it may limit complications from implanted ventricular shunts. |
|
References
- Buckley RT, Yuan W, Mangano FT, et al. Longitudinal comparison of diffusion tensor imaging parameters and neuropsychological measures following endoscopic third ventriculostomy for hydrocephalus. Journal of neurosurgery Pediatrics. 2012;9(6):630-635.
- Di Rocco C, Massimi L, Tamburrini G. Shunts vs endoscopic third ventriculostomy in infants: are there different types and/or rates of complications? A review. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2006;22(12):1573-1589.
- Kulkarni AV, Warf BC, Drake JM, Mallucci CL, Sgouros S, Constantini S. Surgery for hydrocephalus in sub-Saharan Africa versus developed nations: a risk-adjusted comparison of outcome. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2010;26(12):1711-1717.
- Mazzola CA, Choudhri AF, Auguste KI, et al. Pediatric hydrocephalus: systematic literature review and evidence-based guidelines. Part 2: Management of posthemorrhagic hydrocephalus in premature infants. Journal of neurosurgery Pediatrics. 2014;14 Suppl 1:8-23.
- Flannery AM, Mitchell L. Pediatric hydrocephalus: systematic literature review and evidence-based guidelines. Part 1: Introduction and methodology. 2014;14(Supplement_1):3.
- Drake JM, Kulkarni AV, Kestle J. Endoscopic third ventriculostomy versus ventriculoperitoneal shunt in pediatric patients: a decision analysis. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2009;25(4):467-472.
- El-Ghandour NM. Endoscopic third ventriculostomy versus ventriculoperitoneal shunt in the treatment of obstructive hydrocephalus due to posterior fossa tumors in children. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2011;27(1):117-126.
- Kulkarni AV, Drake JM, Kestle JR, Mallucci CL, Sgouros S, Constantini S. Predicting who will benefit from endoscopic third ventriculostomy compared with shunt insertion in childhood hydrocephalus using the ETV Success Score. Journal of neurosurgery Pediatrics. 2010;6(4):310-315.
- Kulkarni AV, Shams I, Cochrane DD, McNeely PD. Does treatment with endoscopic third ventriculostomy result in less concern among parents of children with hydrocephalus? Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2010;26(11):1529-1534.
- Kulkarni AV, Shams I, Cochrane DD, McNeely PD. Quality of life after endoscopic third ventriculostomy and cerebrospinal fluid shunting: an adjusted multivariable analysis in a large cohort. Journal of neurosurgery Pediatrics. 2010;6(1):11-16.
- Sainte-Rose C, Cinalli G, Roux FE, et al. Management of hydrocephalus in pediatric patients with posterior fossa tumors: the role of endoscopic third ventriculostomy. Journal of neurosurgery. 2001;95(5):791-797.
- Shim KW, Kim DS, Choi JU. Simultaneous endoscopic third ventriculostomy and ventriculoperitoneal shunt for infantile hydrocephalus. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2008;24(4):443-451.
- Warf BC, Campbell JW, Riddle E. Initial experience with combined endoscopic third ventriculostomy and choroid plexus cauterization for post-hemorrhagic hydrocephalus of prematurity: the importance of prepontine cistern status and the predictive value of FIESTA MRI imaging. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2011;27(7):1063-1071.
- Appelgren T, Zetterstrand S, Elfversson J, Nilsson D. Long-term outcome after treatment of hydrocephalus in children. Pediatric neurosurgery. 2010;46(3):221-226.
- de Ribaupierre S, Rilliet B, Vernet O, Regli L, Villemure JG. Third ventriculostomy vs ventriculoperitoneal shunt in pediatric obstructive hydrocephalus: results from a Swiss series and literature review. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2007;23(5):527-533.
- Garton HJ, Kestle JR, Cochrane DD, Steinbok P. A cost-effectiveness analysis of endoscopic third ventriculostomy. Neurosurgery. 2002;51(1):69-77; discussion 77-68.
- Kulkarni AV, Drake JM, Kestle JR, Mallucci CL, Sgouros S, Constantini S. Endoscopic third ventriculostomy vs cerebrospinal fluid shunt in the treatment of hydrocephalus in children: a propensity score-adjusted analysis. Neurosurgery. 2010;67(3):588-593.
- Shimizu T, Luciano MG, Fukuhara T. Role of endoscopic third ventriculostomy at infected cerebrospinal fluid shunt removal. Journal of neurosurgery Pediatrics. 2012;9(3):320-326.
- Tuli S, O'Hayon B, Drake J, Clarke M, Kestle J. Change in ventricular size and effect of ventricular catheter placement in pediatric patients with shunted hydrocephalus. Neurosurgery. 1999;45(6):1329-1333; discussion 1333-1325.
- Fani L, de Jong TH, Dammers R, van Veelen ML. Endoscopic third ventriculocisternostomy in hydrocephalic children under 2 years of age: appropriate or not? A single-center retrospective cohort study. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2013;29(3):419-423.
- Jernigan SC, Berry JG, Graham DA, Goumnerova L. The comparative effectiveness of ventricular shunt placement versus endoscopic third ventriculostomy for initial treatment of hydrocephalus in infants. Journal of neurosurgery Pediatrics. 2014;13(3):295-300.
- Kulkarni AV, Sgouros S, Constantini S. International Infant Hydrocephalus Study: initial results of a prospective, multicenter comparison of endoscopic third ventriculostomy (ETV) and shunt for infant hydrocephalus. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2016;32(6):1039-1048.
- Lam S, Harris D, Rocque BG, Ham SA. Pediatric endoscopic third ventriculostomy: a population-based study. Journal of neurosurgery Pediatrics. 2014;14(5):455-464.
- Stone SS, Warf BC. Combined endoscopic third ventriculostomy and choroid plexus cauterization as primary treatment for infant hydrocephalus: a prospective North American series. Journal of neurosurgery Pediatrics. 2014;14(5):439-446.
- Vogel TW, Bahuleyan B, Robinson S, Cohen AR. The role of endoscopic third ventriculostomy in the treatment of hydrocephalus. Journal of neurosurgery Pediatrics. 2013;12(1):54-61.